Gastroesophageal reflux disease, well known as GERD, is a digestive chronic condition whereby acid very often moves back into the esophagus and causes irritation and discomfort. There is a certain code in the ICD that classifies diagnosis for GERD or, in other words, GERD ICD 10. That would help the professionals identify and further treat the disease accordingly. The following paper will elaborate on gastroesophageal reflux disease, outlining its symptoms, causes, available treatments, and the importance of the ICD 10 code.
Read More – Click Here
GERD ICD- 10 What is it?
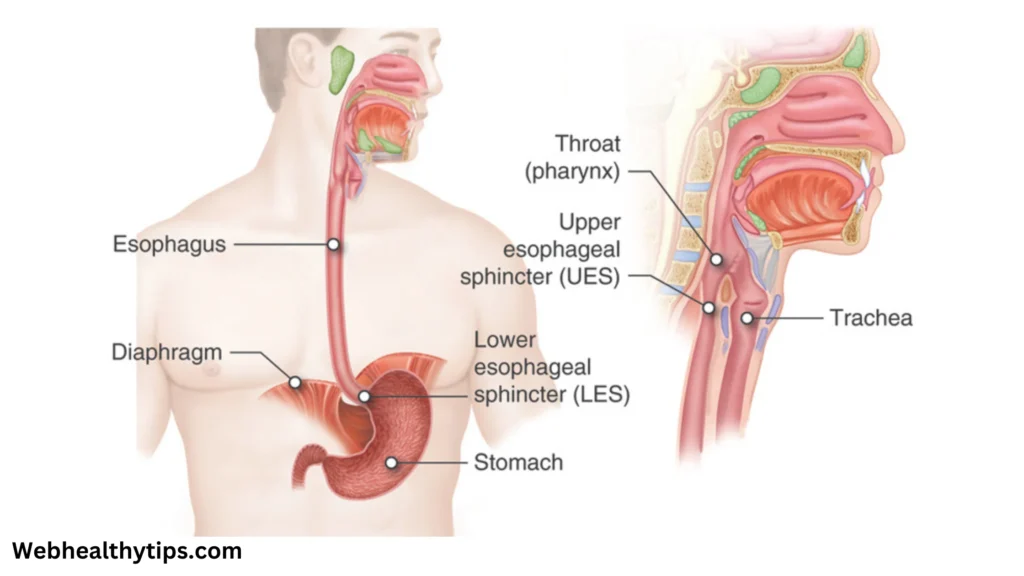
In this disease, the ring of muscle that sits between the esophagus and stomach cannot hold as well; it weakens or relaxes improperly. Stomach acid can then reflux up into the esophagus, causing symptoms such as heartburn. Acid reflux is normal at times; however, gastroesophageal reflux disease is a more serious and long-term illness that requires treatment from a physician.
ICD-10 Code for GE RD
K21.9 is the code for GERD in ICD-10. Without complicating factors, health professionals use the classification for the documentation and diagnosis of GERD. If esophagitis, or inflammation of the esophagus, has set in with GERD, then the ICD-10 code would be K21.0. These codes are important for insurance claims, medical billing, and for applying consistency to treatment regimes.
gastroesophageal reflux disease symptoms
The severity of GERD symptoms varies from person to person and can be moderate to severe. Typical signs and symptoms include of:
- Symptoms of GERD can be differing for each individual; the severity can range from moderate to severe. Common signs and symptoms include:
- Heartburn is a burning sensation in the chest usually produced by eating and often is made worse by lying down.
- Regurgitation involves the sensation of stomach acid or contents reflating backward toward the mouth or throat. Dysphagia-the sensation of food stuck in the esophagus or trouble swallowing.
- Chest pain: This could be caused by acid irritation of the esophagus due to GERD and may be misdiagnosed as a myocardial infarction.
- Chronic Cough: An offended throat due to the backed up acid can result in chronic cough.
- Hoarseness: The contact of acid upsets the vocal cords and can lead to hoarseness.
- Certain individuals feel queasy, especially after eating.
Less noticeable signs would be, for instance, symptoms other than the usual ones that come along with gastroesophageal reflux disease. Heartburn is usually a symptom commonly identified with gastroesophageal reflux disease.
GERD Causes and Risk Factors
This is commonly referred to as GERD – Acid Reflux Disease: Acid reflux disease is a condition where the lower esophageal sphincter, LES, which is tasked with preventing stomach acid from backflowing into the esophagus, either weakens or relaxes too much. Some of the potential development variables for GERD include the following:
Obesity: Being overweight can put pressure on the stomach, forcing acid to reflux into the esophagus.
A hiatal hernia is a condition where the stomach bulges up into the chest through an opening in the diaphragm and shoves the LES downward.
Pregnancy – Gastroesophageal reflux disease symptoms may appear because of hormonal changes and increased abdominal pressure.
Smoking: It can increase the secretion of stomach acids and reduce the quality of LES.
Diet: Foods and beverages, like chocolate, coffee, alcohol, and spicy and/or greasy things, can irritate GERD.
Medications: Many medications, including but not limited to ibuprofen and aspirin, and some blood pressure medicines, may cause direct irritation to the esophagus or result in increased stomach acid.
GERD Diagnosis Using ICD 10 Code
Use ICD code K21.9 for the diagnosis of GERD when there are no specific issues such as esophagitis. In contrast, code K21.0 is assigned when GERD is associated with injury or inflammation of esophagus. The ICD 10 code is useful for:
Medical Record-Keeping: Physicians can successfully track the diagnosis and treatment outcomes of GERD by using the ICD 10 code for proper record-keeping.
Insurance and Billing: In order to guarantee that patients receive the proper coverage for GERD-related medical care, the ICD 10 code is crucial for insurance claims and reimbursement.
Clinical Research: ICD codes are used by academics and medical facilities to find patterns, treatment results, and patient information for GERD and other condition-related studies.
Techniques for Diagnosing gastroesophageal reflux disease

Clues in history combined with diagnostic testing are useful but empiric therapy is often initiated without any further evaluation. Standard techniques include:
Endoscopy: A flexible tube with a camera is inserted down the esophagus to assess for any inflammation or other disorders.
pH monitoring – used to measure acid in the esophagus, and needed with an age determination of reflux.
Esophageal Manometry: Measures the pressure and function of the LES and the esophagus to ensure these are working properly.
Barium Swallow: This is a procedure in which patients drink a solution with barium in it so that the esophagus can be seen more clearly on an X-ray, thereby helping to identify any abnormalities.
GERD Treatment Options
Depending on the degree of symptoms, gastroesophageal reflux disease can be managed with a variety of therapy methods. Treatment options include medication, lifestyle changes, and occasionally surgery.
Changes in Lifestyle
However, making certain lifestyle changes can progressively decrease the symptoms of GERD. Among them are:
Diets: Avoid food that causes acid attacks which include those that are acidic, fat and of spices.
Weight control: if someone is overweight & carrying extra pounds, particularly in their midsection,the pressure on their stomach creates added acid flow which encourages heartburn(progesterone hormone released during pregnancy also causes the valve between the esophagus and stomach to relax).
Elevate the Head of the Bed: Sleeping with your head elevated can reduce nighttime reflux.
Quit smoking: Smoking can weaken the LES; consequently quitting can potentially reduce your symptoms.
Small Meals- If you eat smaller but more meals, this may prevent your stomach from producing TOO much acid.
Drugs used to treat GERD

Prescription drugs are often used to smooth the symptoms of gastroesophageal reflux disease and to prevent any further deterioration of esophageal damage and include:
Antacids: Over-the-counter antacids neutralize acid reflux and offer immediate relief.
H2 Blockers: These prescription drugs, including ranitidine (Zantac) and famotidine (Pepcid), are designed to decrease acid production in the stomach and provide longer term relief of symptoms.
Proton Pump Inhibitors (PPIs) Intense drugs that inhibit acid secretion and accelerate healing of oesophagitis: omeprazole, esomeprazole.
Prokinetics: These drugs help strengthen the LES and encourage the stomach to empty faster, thus reducing the risk of reflux.
Surgical Techniques

Patients with GERD who do not respond to lifestyle changes or medications could be candidates for surgery. Surgical procedures include:
Nissen Fundoplication: the surgeon wraps the upper portion of the stomach around the lower esophagus to help strengthen the LES. This stops acid reflux.
LINX Device: Food passes through the LES while acid reflux is prevented by a small circle of magnetic beads that is placed around it.
The Stretta Procedure is a minimally invasive procedure where radiofrequency energy is used to strengthen the muscles of the LES.
Possible Side Effects of Untreated GERD
Untreated GERD can result in a number of problems, such as:
Esophagitis: Constant exposure to acid causes inflammation of the lining of the esophagus.
Esophageal Stricture: The integration of scar tissue in the esophagus causes narrowing of the esophagus and dysphagia.
The cells that line the oesophagus also change in Barrett’s esophagus, a pre-cancerous condition that makes the patient more at risk of oesophageal cancer.
Trouble breathing: The inhalation of stomach contents from a chronically refluxed stomach can lead to trouble breathing, such as pneumonia or asthma.
In summary
A common and potentially dangerous digestive disorder that can have a major negative influence on quality of life is GERD. One of the most important ICD 10 codes for GERD (K21.9) is used in its diagnosis, documentation, and treatment. Patients can effectively manage their GERD and avoid complications by working with their healthcare providers to understand the symptoms, causes, and available treatment choices.
Changing one’s lifestyle, taking prescription drugs as directed, and getting help when needed are essential for controlling GERD symptoms and preserving digestive health. In order to receive the proper diagnosis and treatment, you should always speak with a healthcare provider if you think you might have GERD.